Joining 1 and 2 gives the line for identifying the individual vertebrae, the transverse processes of which lie just posterior to the line.
Fig. 75:1. Courtesy of Astra.
1. Mastoid process
2. Sternomastoid muscle
3. Transverse process of C6
Fig. 75:2.
1. Posterior primary ramus
2. Anterior primary ramus
3. Grey ramus communicans
4. Vertebral artery
5. Superior cervical ganglion
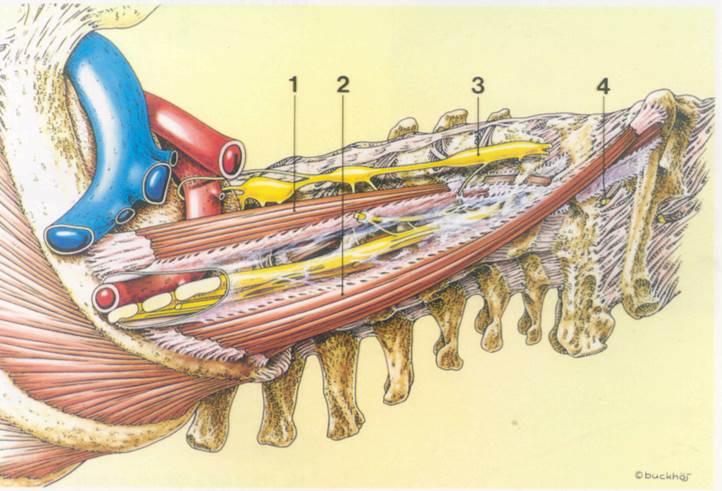
Fig. 75:3.
1. Scalenus anterior muscle
2. Scalenus medius muscle
3. Sympathetic chain
4. Spinal root Cl
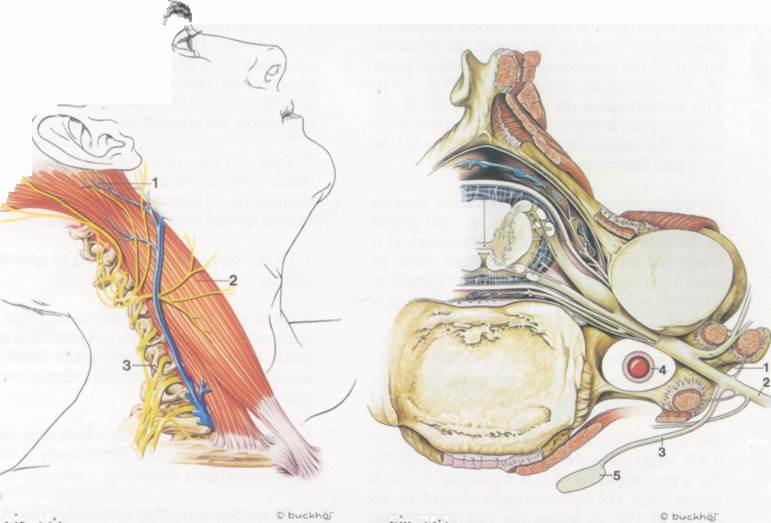
Fig. 75:1. Fig. 75:3.
Fig. 75:2.
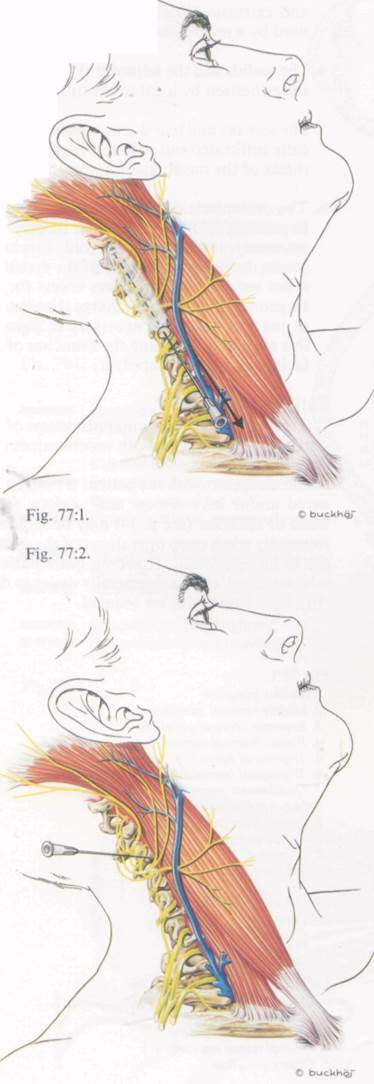
Needle insertion
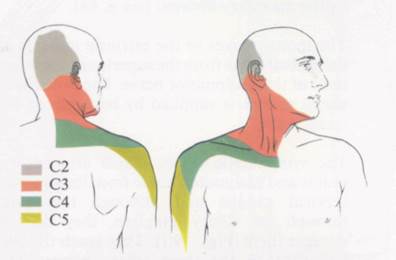
For a superficial block, the subcutaneous tissues are infiltrated in the line of the posterior border of the sternomastoid, the central point of the infiltration being at C3-4 (Fig. 77:1). This anaesthetises the skin only, in the distribution of the lesser occipital, the greater auricular, the transverse cutaneous nerve of the neck and the supraclavicular nerves.
For a deep block, the needle is directed towards the transverse processes of C3, at right angles to the skin and pointing slightly caudad. It is advanced 1.5-3 cm so as to contact bone or elicit a paraesthesia. The needle hub should be carefully examined for escape of blood or cere-brospinal fluid (Fig. 77:2 and 77:4).
Drugs and dose
For a superficial block, 10 ml of 1% lidocaine or 0.25% bupivacaine on each side.
For a deep block, 10 ml of 2% lidocaine or 0.5% bupivacaine (with epinephrine 1:200.000 for a prolonged block). If a bilateral block is being done, the concentration should be reduced to 1%, to lessen the risk of bilateral phrenic paralysis.
Complications
1. Subarachnoid injection leading to a high spinal block. The patient will usually become unconscious and may stop breathing. Severe hypotension may also occur. Treatment consists of artificial ventilation and a vasopressor to support the circulation.
2. Epidural injection which will cause anaesthesia in the upper limbs and thorax. Unlike a subarachnoid injection, the local anaesthetic cannot spread into the cranium.
3. Intravenous injection leading to generalised toxicity.
4. Intra-arterial injection due to the close proximity of the vertebral artery. As the local anaesthetic drug will go direct to the brain, very small quantities can cause convulsions and apnoea.
5. Phrenic nerve paralysis which may lead to respiratory difficulties, particularly if there is pre-existing lung disease.
6. Anaesthesia of other nerves in the neck such as the vagus, glossopharyngeal and cervical sympathetic chain. This can cause hoarseness (due to recurrent laryngeal nerve block), difficulty in swallowing, Horner's syndrome, etc.
Suggested further reading
Evers, H. & Haegerstam, G (1981) Handbook of Dental Local Anaesthesia, Schultz, Copenhagen.
Gautier-Lafaye, P. (1985) Laco-regional anaesthesia for the head & neck. In Precis d'Anesthesie Loco-Regionals. Masson, Paris, p. 47.
77:1, 2 and 3. Courtesy of Astra.
I ... n.noj
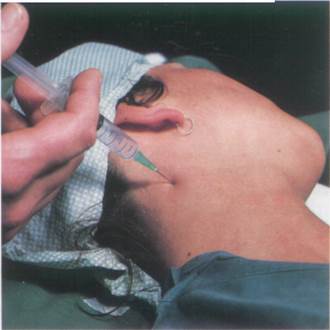
Fig. 77:3. Fig. 77:4.
Local anaesthesia in ophthalmology
Anatomy *
The somatic sensory nerves to the eyeball run in the long ciliary nerves which derive from the nasociliary nerve, a branch of the ophthalmic nerve (Fig. 79:2). The sensory nerves to the upper eyelid and adjacent skin also come from the ophthalmic division of the trigeminal nerve (Fig. 57:2), while the lower lid is supplied by the maxijlary division (see p. 64).
The motor nerves to the extrinsic muscles of the eyeball come from the superior and inferior rarni of the oculomotor nerve. The orbicularis occuli muscle is supplied by branches of the facial nerve.
The sympathetic fibres, which are sensory, motor and vasomotor, come from the superior cervical ganglia and although they pass through the ciliary ganglion, they do not synapse there (Figs. 79:1). They reach the eyeball through the short ciliary nerves. The motor fibres supply the dilator pupillae muscle.
The parasympathetic supply comes from the oculomotor nerve and the fibres enter the ciliary ganglion, where they synapse. The post-ganglionic fibres run in the short ciliary nerves and supply the constrictor pupillae muscle (Fig. 79:1).
The eyeball, including its intrinsic and extrinsic muscles, can be blocked by injecting local anaesthetic into the cone formed by the extrinsic muscles, close to the ciliary ganglion i.e. a retrobulbar injection.
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.