This simple block will allow all types of reconstructive surgery on the eyelid. It should be remembered that the infiltration will swell the lid and it may be difficult to locate, say, a tarsal cyst unless it has been identified and marked before the injection.
Drugs and dose
4-5 ml of 0.5 or 1% lidocaine or its equivalent (see p.-20).
Conjunctiva
Infiltration of the conjunctiva (after iniual topical anaesthesia) will allow operations such as cryocoagulation of the retina. The anaesthetic is deposited just behind the insertion of the rectus muscle, i.e. where the retina ends.
Drugs and dose
1-3 ml of 0.5% lidocaine or its equivalent 1see p. 20).
Tear sac and tear ducts
A needle is inserted 0.5 cm above the medial canthus and directed backwards and medially until it contacts the orbital septum. 0.5 ml of local anaesthetic is injected and the needle redirected more medially to contact the medial wall of the orbit, above the medial paipebral ligament, where a further 0.5 ml is injected. These injections are repeated in relation to the lower eyelid, the needle penetrating the orbital septum just below the medial paipebral ligament (Fig. 83:2).
The nasal mucous membrane is anaesthetised by spraying the nose and applying gauze soaked in local anaesthetic (see p. 36).
Drugs and dose
2 ml of 0.5 % lidocaine or its equivalent for the injection, and 5 ml of 4% lidocaine for the nasal mucous membrane. Operative bleeding will be greatly reduced by adding epinephrine, 1:200.000, to the injection and 0.25 ml of 1:1.000 (250 jug) to the topical solution.
Figs. 83:1 and 2. Courtesy of Astra.
Fig. 83:1.
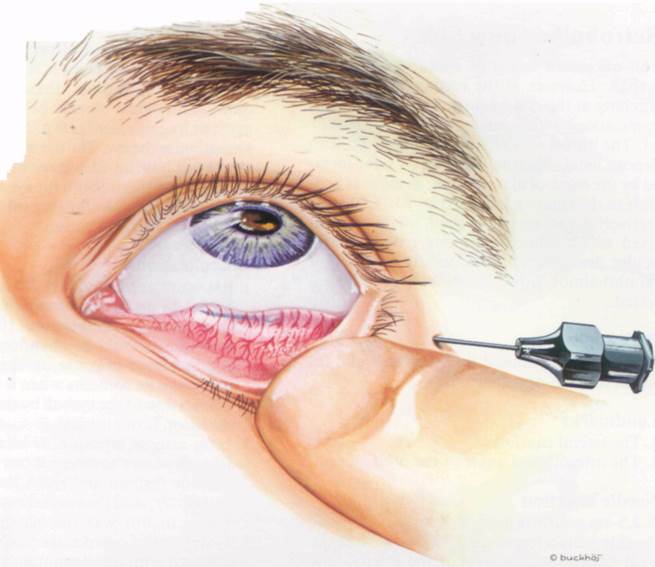
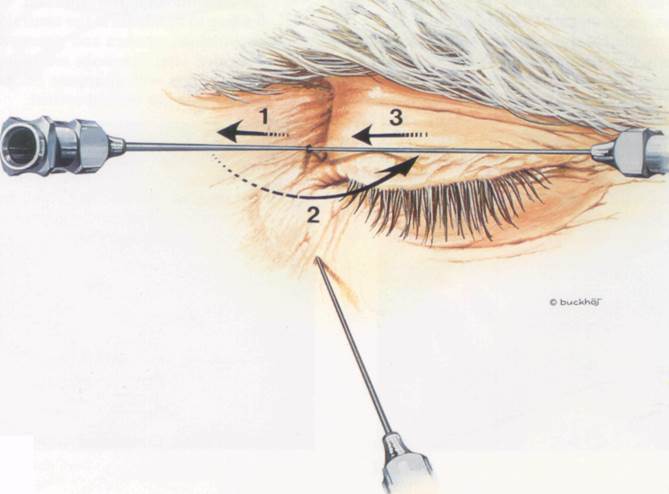
Fig 83:2.
83
Retrobulbar injection
This allows all forms of operation upon the eyeball. However, if the conjunctiva requires stitching at the end of surgery, further topical application or local infiltration may be required. The object of a retrobulbar injection is to deposit local anaesthetic within the cone formed by the extra-ocular muscles, as close as possible to the ciliary ganglion (Fig. 85:1). This effectively denervates the eyeball, leaving it paralysed with a dilated pupil and reduced intraocular pressure. There is usually a degree of exophthalmos from the volume of fluid injected.
Patient position
Supine. Patient should look upwards and towards the non-operated side.
Landmarks
1. The lateral canthus
2. The inferolateral angle of the orbit
Needle insertion
A 3.5-cm needle is used. It is inserted through the skin 1 cm below and 0.5 cm medial to the lateral canthus at the level of the inferolateral angle of the orbit (Figs. 85:2 and 85:3). It is directed medially, superiorly and posteriorly towards the apex of the orbit. The eyeball may be gently retracted medially with the forefinger of the non-dominant hand. To push away structures, particularly blood vessels, in the path of the needle, local anaesthetic should be injected slowly but continuously as the needle is advanced. The orbital septum of the lower eyelid will be felt as it is pierced. The needle is inserted to its full 3.5 cm (Fig. 85:4). After careful aspiration, the main injection'is made. 5 min should be allowed for the block to become fully effective. The application of a tight pressure dressing to the eye aids diffusion of the local anaesthetic.
Drugs and dose
To allow the maximum effect from a small volume of local anaesthetic, it is necessary to use higher concentrations than in the other ophthalmological blocks. 2-3 ml of 2% lido-caine or its equivalent (see p. 21) is sufficient to anaesthetise the eye. The use of a larger volume (10-12 ml) has the advantage of spreading the drug to anaesthetise both the eye and the orbic-ularis oculi muscle allowing intra-ocular surgery with a single injection.
Complications
1. Retrobulbar haematoma. This will be diagnosed by increasing exophthalmos in the first minutes after injection. If it occurs, the operation should be abandoned otherwise the increased pressure on the eyeball may discharge its contents when it is opened.
2. Transfixion of the eyeball by the needle if the direction is too medial.
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.