3. Intra-arterial injection. If local anaesthetic is injected into an artery, it can travel in a retrograde fashion and reach the internal carotid artery and thus gain direct access to the brain. In this way the classical signs and symptoms of overdosage (see p. 22) can occur even with small amounts of drug.
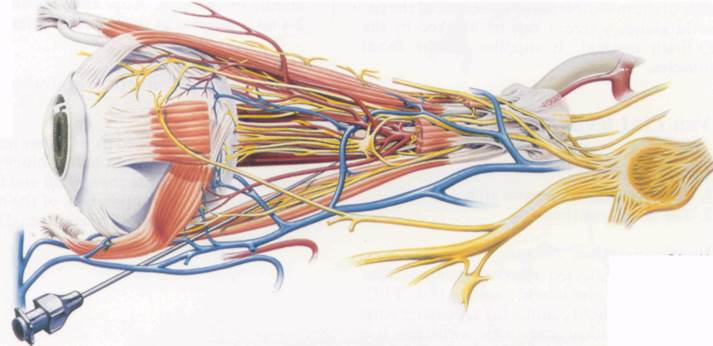
4. Subarachnoid injection. A dural cuff containing cerebrospinal fluid surrounds the optic nerves and may be entered by the needle. Local anaesthetic can then reach the optic chiasma and the adjacent structures, leading to blindness in the contralateral eye, convulsions, apnoea and unconsciousness. Provided vital functions are supported, all these effects will disappear once the local anaesthetic has been absorbed.
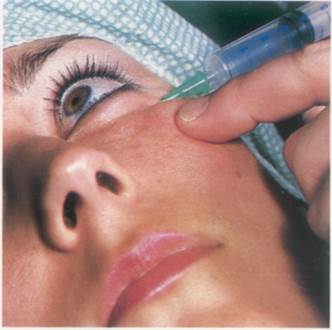
Injection into the optic nerve covrings requires a relatively high pressure and the injection should be stopped if resistance is encountered. Before attaching the syringe, small movements of the needle will cause the eyeball to move if the nerve has been entered.
Figs. 85:1 and 2. Courtesy of Astra.
84
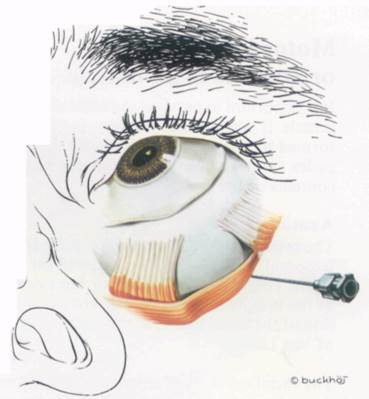
Fig. 85:3.
Fig. 85:2.
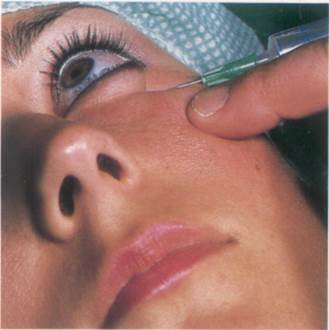
Fig. 85:4.
85
Fig. 85:1.
Motor blockade of the orbicularis oculi muscle
It is important to paralyse the orbicularis oculi muscle if intra-ocular surgery is being performed to prevent blepharospasm, which impedes surgical access and may discharge the contents of the eye.
Anatomy
The orbicularis oculi muscle is supplied by the temporal and zygomatic branches of the facial nerve. These cross the zygomatic bone en route to the muscle and can be blocked by infiltration of the facial tissues in this area (technique of Van Lint).
The facial nerve itself enters the face through the stylomastoid foramen and crosses the con-dyle of the mandible in the substance of the parotid gland, where it can be blocked by the O'Brien method. It supplies all the facial muscles.
Van Lint technique
Landmarks
1. The zygomatic bone and arch
2. The lateral canthus
Needle insertion
The needle is inserted over the zygomatic bone 2-3 cm below the lateral canthus (Fig. 87:1). The needle should contact the zygomatic bone where 2 ml of local anaesthetic is injected. It is then directed upwards and laterally to pass 1 cm behind the lateral canthus, within the deep tissues. As it is withdrawn, 2-3 ml of local anaesthetic is injected. On reaching the subcutaneous tissue, the needle is redirected at right angles parallel to the inferior margin of the orbit, and a further 2-3 ml injected on withdrawal. Some authorities also inject along the superior margin of the orbit.
Drugs and dose
6-8 ml of lidocaine 1% or its equivalent (see p. 20).
O'Brien technique
Landmarks
1. The condyle of the mandible
2. The tragus of the ear
3. The zygomatic arch
Needle insertion
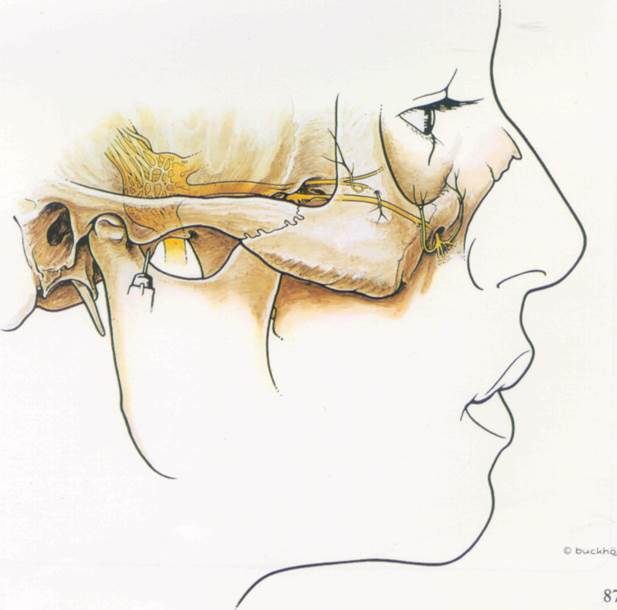
The needle is inserted perpendicularly to the skin towards the mandibular condyle just in front of the tragus (Fig. 87:2). After contacting the condyle, the needle is slowly withdrawn as 2-4 ml of local anaesthetic is injected. This should block the nerve but the blockade may be reinforced by further injections through the same puncture site, the needle being directed first vertically, then towards the anterior part of the zygomatic arch and finally towards the middle of the arch. After each advancement 2-4 ml is injected as the needle is withdrawn.
Drugs and dose
8-16 ml of 1% lidocaine or its equivalent (see p. 20).
As previously mentioned (p. 84) some authorities use a large volume retrobulbar block alone, which will anaesthetise the eyeball and the orbicularis oculi. Motor paralysis of the muscle is easily tested and should be confirmed before starting surgery.
Fig. 87:1. Courtesy of Astra.
86
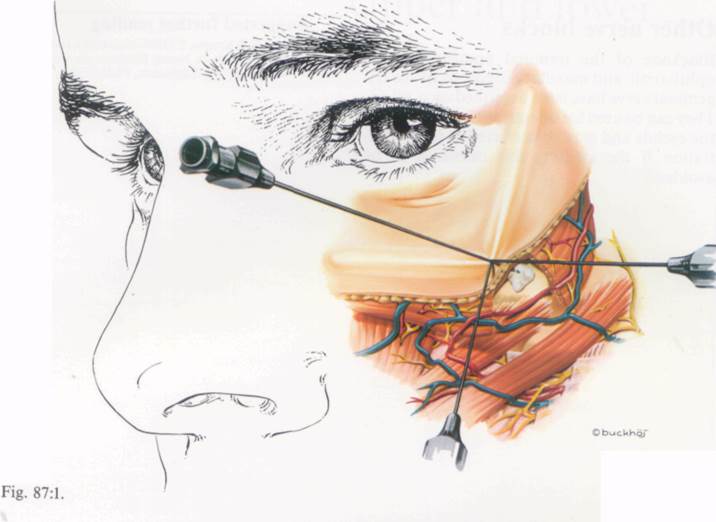
Fig. 87:2.
Other nerve blocks
Blockade of the terminal branches of the ophthalmic and maxillary divisions of the tri-geminal nerve have been described on p. 60-65. They can be used for operations on and around the eyelids and may be preferred to local infiltration if the swelling this causes is to be avoided.
Suggested further reading
Feitl, M.E. & Krupin, T. (1988) Neural blockade for ophthalmo-logic surgery. In Neural Blockade eds Cousins M.J. & Bri-denbaugh, P.O. Lippincott, Philadelphia, p. 577.
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.