Principles
To perform painless surgery in ophthalmologi-cal practice, it is necessary to consider the eye and its surrounding tissues as six separate components, namely:
1. The cornea, which is easily anaesthetised by topical local anaesthesia
2. The conjunctiva, which is more difficult to anaesthetise topically but can additionally be anaesthetised by local infiltration or nerve blockade
3. The eyeball itself (together with the intrinsic and extrinsic muscles), which is anaesthetised by a retrobulbar injection
4. The eyelids and the adjacent skin, which are anaesthetised by local infiltration
5. The tear sac and tear ducts, which can be locally infiltrated but will also require anaesthesia of the nasal mucosal membrane
6. The orbicularis oculi muscles, which must be paralysed during intraocular surgery. It is extremely important to avoid blepharo-spasm during open surgery of the eyeball as it not only seriously hinders access for the surgeon, but can also discharge the contents of the eye. Thus it is necessary to paralyse this muscle by blocking the branches of the facial nerve which supply it.
Patient management
It is very important to avoid restlessness of the patient, which can be both inconvenient and dangerous.
Good rapport with the patient is essential to avoid undue nervousness and anxiety. Some form of sedation (see p. 14) may be required, especially when open operations of the eyeball are to be performed. However, older patients who are unsedated, are generally easier to deal with than those who are sedated.
Fig. 79:1.
1. Stellate ganglion
2. Middle cervical ganglion
3. Superior cervical ganglion
4. Plexus internal carotid
5. Trigeminal nerve (V)
6. Tftgeminal (seminular) ganglion
7. Oculomotor nerve (III)
8. Nasociliary nerve
9. Long ciliary nerves
10. Ciliary ganglion
11. Cornea
12. Sphincter pupillae muscle
13. Iris
14. Dilatator pupillae muscle
15. Vas
16. Ciliaris muscle
17. Ciliary body
Fig. 79:2. Courtesy of Astra. /. Inferior ophthalmic vein
2. Inferior oblique muscle
3. Lateral rectus muscle
4. Inferior rectus muscle
5. Ciliary ganglion
Fig. 79:1.
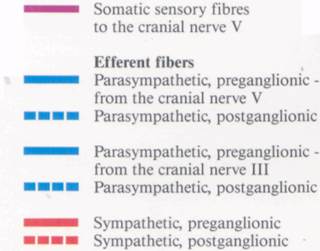
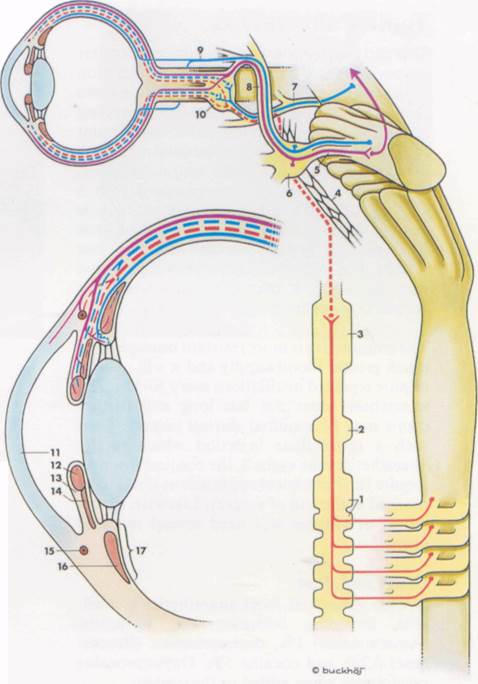
Fig. 79:2.
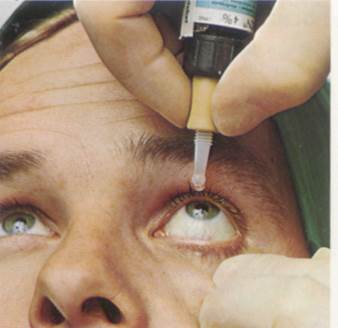
Topical anaesthesia
This can be used for virtually all simple ocular manoeuvres and should precede any injection of the conjunctiva. The eye cannot retain more than about 1 drop of fluid, any excess running out onto the face. Thus only a limited amount of local anaesthetic can be absorbed after each instillation, regardless of the amount instilled. The cornea is usually anaesthetised with a single instillation, but the patient should be warned that all local anaesthetics sting a little on their first instillation, and this may last 15-30 s. If a second or subsequent application does not sting, it may be assumed that the cornea is anaesthetised.
The conjunctiva is more resistant because of its much greater blood supply and it will usually require repeated instillations every 30-45 s. The anaesthesia does not last long and further drops may be required during surgery. Even with a retrobulbar injection which totally anaesthetises the eyeball, the conjunctiva may require further topical applications if it is to be stitched at the end of surgery. Likewise, the removal of stitches will need several repeated drops.
Drugs and dose
A wide variety of local anaesthetics is available, including lidocaine 4%, tetracaine (Amethocaine) 1%, oxybuprocaine (Benoxi-nate) 0.2% and cocaine 5%. Oxybuprocaine precipitates when added to fluorescein.
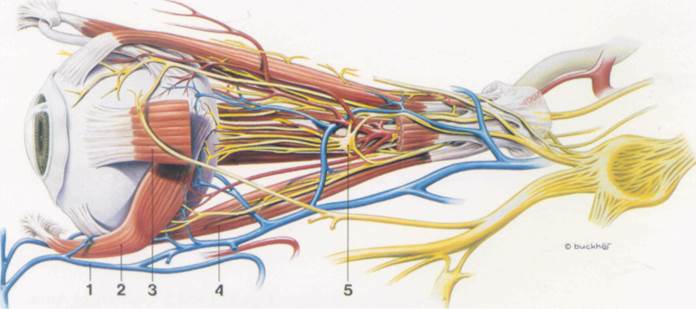
Figs. 81:1 and 2. Courtesy of Astra.
Fig. 81:1.
Fig. 81:2.
Local infiltration
This can be used for operations on the eyelids (and/or the adjacent skin), the conjunctiva and the tear sac and ducts.
Eyelids
To anaesthetise the eyelids, topical local anaesthetic is firsLapplied to the conjunctiva. The eyelid (upper or lower) is everted and a fine needle inserted into the conjunctiva at the lateral part of the lid and advanced along its whole length, injecting as the needle is moving (Fig. 83:1). The needle is withdrawn back to its point of insertion, and while still in the sub-conjunctival tissue, the eyelid is inverted to its normal position. The needle is then turned outwards and pushed through the orbital septum to enter the subcutaneous aspect of the eyelid. Local anaesthetic is then deposited along the length of the lid subcutaneously.
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.