The mental foramen is palpated just posterior to the first premolar tooth 1 cm below the gum margin.
Needle insertion
The needle is inserted 1 cm below the first premolar directed backwards and medially to contact the bone near the foramen but not to enter it (Fig. 71:2).
Transcutaneous approach
The mental foramen is palpated through the skin and a needle is directed upwards, medially and backwards to contact the mandible at the foramen (Fig. 71:3).
Drugs and dose
1-1.5 ml of 2% lidocaine with adrenaline 1:80.000 or 3% prilocaine with felypressin (Octapressin) 0.03 lU/ml.
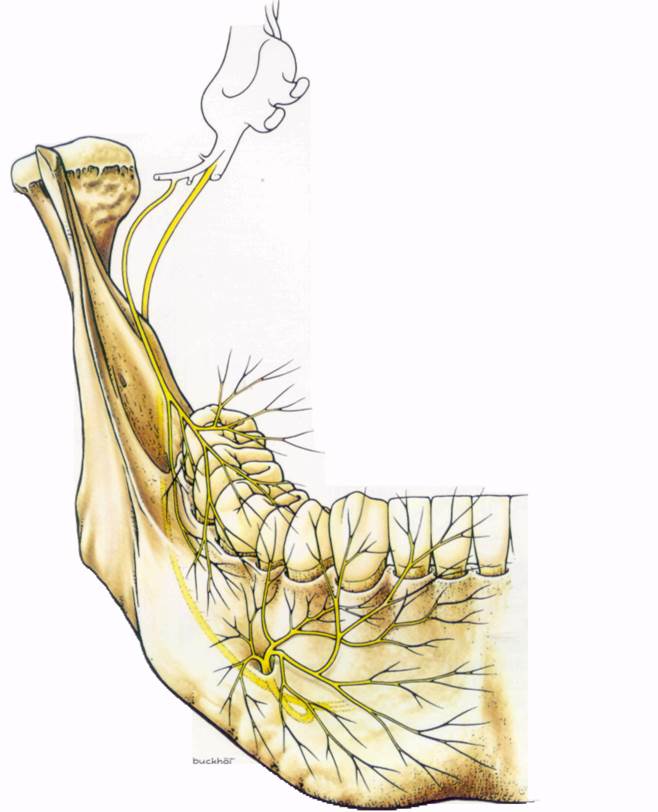
Fig
Fig. 71:2.
Fig. 71:3.

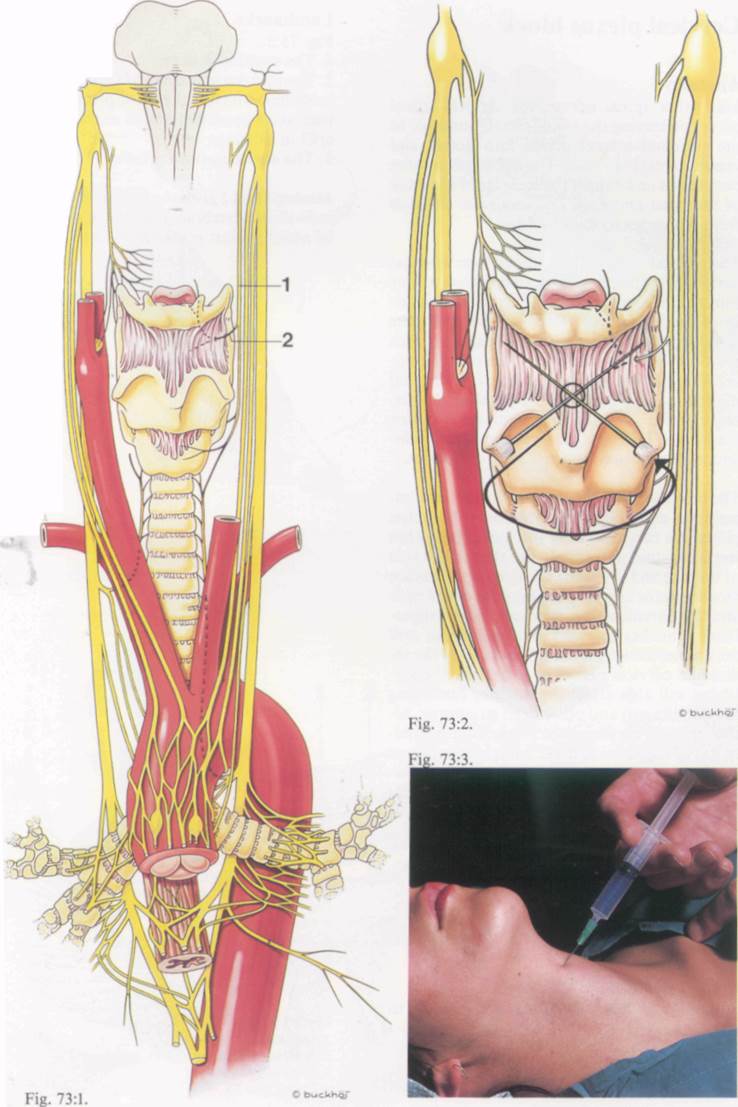
Superior laryngeal nerve block
Anatomy
An aid to anaesthetising the larynx is by superior laryngeaj nerve block (Fig. 73:1). This nerve, a branch of the vagus nerve, runs behind the greater cornu of the hyoid bone where it divides into the internal and external laryngeal nerves. The former pierces the thyrohyoid membrane midway between the thyroid and hyoid bones to provide the sensory innervation to the larynx and the lower pharynx including the epiglottis. The external laryngeal nerve supplies the cricothyroid muscle and the inferior constrictor of the pharynx.
For topical anaesthesia of the larynx see page 34. .
Patient position
Supine or sitting up.
Landmarks
1. Thyroid cartilage
2. Hyoid bone (greater cornuae)
Needle insertion
Using a median approach (Figs. 73:2 and 73:3), a needle is inserted at the upper border of the thyroid bone and directed laterally and superiorly towards the posterior part of the greater cornu of the hyoid bone using the index finger to guide it.
Alternatively, using a lateral approach two injections can be made, one on each side, just inferior to the posterior part of the greater cornuae.
Drug and dose
2-3 ml of 2% lidtocaine or its equivalent (see p. 21) will block each nerve. The injection is then repeated on the opposite side. This will render the larynx anaesthetic without gross impairment of the muscles of the larynx which are supplied by the recurrent laryngeal nerves, and are unaffected by this block.

Fig. 73:1.
/. Superior laryngeal nerve
2. Internal laryngeal nerve
73
Cervical plexus block
Anatomy
Like other spinal nerves, the cervical spinal nerves on leaving the spinal canal (posterior to the vertebral artery) divide into dorsal and ventral rami (Fig. 75:2). The dorsal rami curve backwards and supply the muscles of the back of the head and neck and innervate the skin from the vertex to the shoulders.
The ventral rami of the upper four cervical nerves form the cervical plexus (the lower four join the brachial plexus). This plexus innervates the skin of the front of the neck, the shoulders and the upper chest, together with the neck muscles. The plexus lies over the upper four cervical vertebrae, deep to the internal jugular vein and the sternomastoid muscle, and anterior to the scalenus medius and levator scapulae (Fig. 75:1). There is considerable intercommunication between adjacent nerves.
The branches of the plexus are divided into superficial and deep. The superficial branches pierce the cervical fascia just posterior to the sternomastoid and supply the skin of the side of the face and the neck. The deep branches are mostly motor nerves to the muscles of the neck and the phrenic nerve. Blockade of the superficial branches is easily performed but will only anaesthetise the skin. Blockade of the individual cervical nerves as they leave the vertebrae will also affect the muscles (including the diaphragm) and other deep structures. Although each nerve may be blocked individually, it is much easier to make a single injection at C3. Because local anaesthetic spreads paraver-tebrally quite readily, C2 and C4 will be blocked together with C3. - '
Indications for cervical plexus block are:
1. Superficial operations on the neck and shoulders
2. Operations on the thyroid gland
3. Pain therapy
Patient position
Supine with head extended and turned to opposite side.
Landmarks
Fig. 75:3.
1. The mastoid process
2. The transverse process of C6 (Chassaignac's tubercle), which is the most prominent of the transverse processes and is at the level of the cricoid cartilage
3. The sternomastoid muscle
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.