2. Vertebral artery
3. Sternomastoid muscle
4. Common carotid artery
5. Stellate ganglion
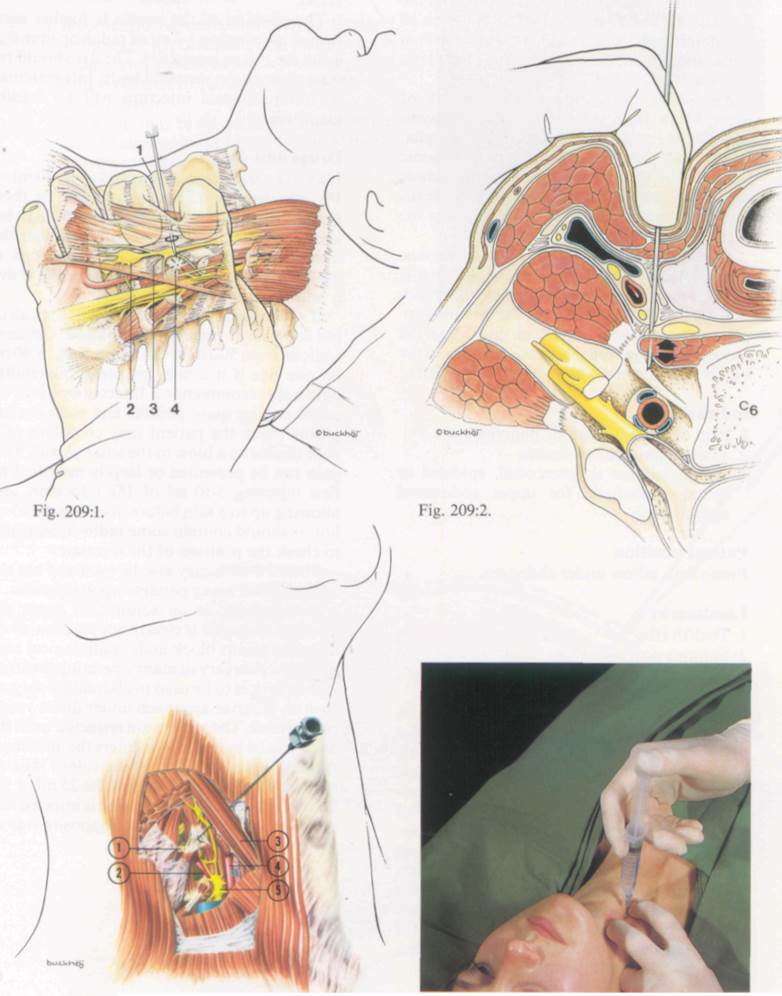
Fig. 209:3. Fig. 209:4.
Coeliac plexus block
Anatomy
The coeliac plexus is situated retroperitoneally in the upper abdomen. It is at the level of the T12 and LI vertebrae, anterior to the crura of the diaphragm. It surrounds the abdominal aorta and the coeliac and superior mesenteric arteries.
The plexus is composed of a network of nerve fibres, both sympathetic and parasym-pathetic. It contains two large coeliac ganglia, one on each side, which receive preganglionic sympathetic fibres from the three splanchnic nerves (greater, lesser and lowest). The plexus also receives parasympathetic fibres from the vagus nerve.
Connected to the coeliac plexus are numerous secondary plexuses such as the hepatic, gastric, splenic, renal, and suprarenal. From these are derived much of the autonomic supply to the abdominal viscera, including the kidneys and suprarenal glands, as well as to the blood vessels which supply them (Fig. 211:1).
Indications
1. Pain of acute or chronic pancreatitis.
2. Visceral pain due to cancer.
3. As an adjunct to intercostal, epidural or spinal anaesthesia for upper abdominal operations.
Patient position
Prone with pillow under abdomen.
Landmarks
1. Twelfth ribs
2. Spinous process of L2
Needle insertion
A 10-15 cm 18 or 20 gauge needle is used. A skin wheal is raised 8 cm lateral to the midline at the lower border of the 12th rib. This should be at the level of the LI vertebra. The needle is inserted medially at 45°so as to miss the transverse spinous process and contact the body of the LI vertebra. It is then withdrawn and reinserted a little steeper so as to glide past the vertebral body. After advancing slowly for 2-3 cm, the needle position should be checked radiolo-gically. The tip should be 1-2 cm anterior to the vertebral body in a lateral view and within the lateral border of the body in an anteropost-erior view (Figs. 211:2 and 211:3).
Because the aorta (left side) and the inferior vena cava (right side) are close to the coeliac plexus, a constant watch should be kept for blood escaping from the needle hub (Fig. 211:4).
The position of the needle is further confirmed by injecting 1-2 ml of radio-opaque dye using the image intensifier. The dye should remain close to the vertebral body. Intravascular or intraperitoneal injection will be readily identified.
Drugs and dose
If local anaesthetic is to be used, then 20 ml of 1% lidocaine or 0.25% bupivacaine or their equivalent should be injected. It is usual to inject the coelic plexus bilaterally although the injectate can cross the midline if enough is used. This can be checked radiologically if dye is added to the local anaesthetic.
If a neurolytic agent is to be used, then alcohol is the most frequently employed. Concentrations from 50-100% (20 ml per side, or 40 rnl on one side if it is seen to spread bilaterally) have been recommended. Injected by itself, alcohol can be quite painful and with coeliac plexus block the patient may complain of a pain similar to a blow to the solar plexus. This pain can be prevented or largely modified by first injecting 5-10 ml of 1% lidocaine, and allowing up to 5 min before injecting the alcohol. It should contain some radio-opaque dye to check the position of the injectate.
Phenol 6-10% may also be used and has the advantage of being painless upon injection.
If being used as an adjunct for upper abdominal surgery it is clearly not practical to do a coeliac plexus block under radiological control before surgery in many operating theatres. If the block is to be used in abdominal surgery then an anterior approach under direct vision can be used. The viscera are retracted until the aorta can be palpated as it enters the abdomen. A needle is inserted close to one side of the aorta so as to contact the vertebra. 20-25 ml of 1% lidocaine or 0.25% bupivacaine is injected and the injection repeated on the opposite side of the aorta.
Complications
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.