2. Absence of sweating in the same area.
3. Constriction of the pupil.
4. Ptosis of the upper eyelid.
The system also supplies many other structures, including the heart, the pharynx, the thyroid and the carotid body, but effects on these structures would only be evident with a bilateral block, which is not recommended.
(2), (3) and (4) above are components of Hor-ner's syndrome, which appears with a successful stellate ganglion block.
Indications
Stellate ganglion block has been used for a wide variety of conditions, including:
1. Raynaud's phenomenon
2. Causalgia or other reflex sympathetic dystrophies in the upper limb
3. To relieve arterial vasoconstriction in the upper limb, e.g. following intra-arterial injection of thiopental, frpstbite or following microsurgical operation
4. Herpes zoster
5. Hyperhidrosis
Because a single injection of local anaesthetic will only have a short-lived effect, it is necessary to reblock the stellate ganglion at frequent intervals to try to break the vicious circle causing the pain. A catheter technique similar to that of epidural block can be used for continuous blockade.
The use of neurolytics is generally inadvisable due to the proximity of the brachial plexus and the phrenic nerves, not to mention other important structures in the neck. Stellate ganglion block has been used as a predictor of effect prior to surgical excision of the ganglion, but this is a potentially very hazardous operation.

Fig. 206:1.
/. First rib
2. Subclavian vein
3. Subclavian artery
4. Stellate ganglion
5. Anterior scalene muscle
6. Middle scalene muscle
7. Transverse process of C6
206

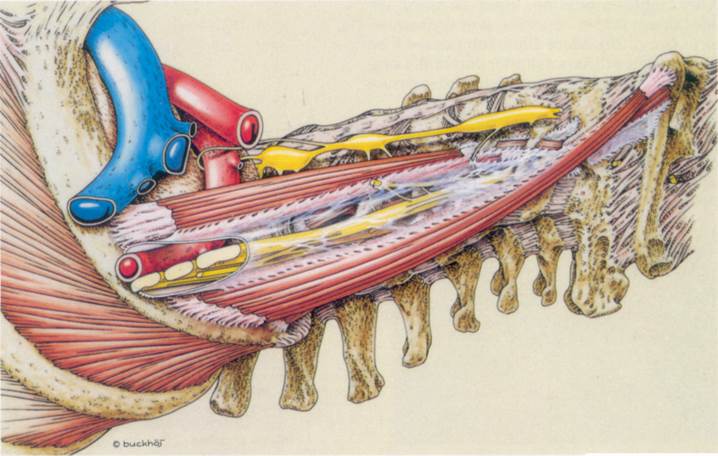
Fig. 207:2.
,^<*^~
Fig. 207:1.
Patient position
Supine with head raised and extended, as for endotracheal intubation.
Landmarks
1. The cricoid cartilage (which is at the level of the 6th cervical vertebra) and the trachea
2. The sternomastoid muscle
3. The carotid artery
4. The transverse'process of C6, felt by palpating between (2) and (3) laterally and (1) medially
Needle insertion
Using two fingers of the non-dominant hand to palpate the transverse process and to hold the skin immobile, a short (4-cm) 22 gauge needle is inserted between the trachea medially ,and the sternomastoid and carotid artery laterally (Fig. 209:1). It is directed perpendicularly backwards until it contacts bone (the transverse process of C6). If it meets resistance which is not clearly bony, it may be in contact with the interspinous ligament or the insertion of the longus colli muscle (Fig. 209:2). It should be withdrawn and reinserted until bone is felt. The needle is then withdrawn 1-2 mm and held firmly while an assistant attaches a flexible cannula and syringe (Figs. 209:3 and 209:4).
Drugs and dose
After careful aspiration, inject 10 ml of 1% lidocaine or 0.25% bupivacaine or their equivalent (see p. 20). More dilute solutions will be effective but will have a shorter duration. Larger doses (up to 20 ml) may be required to ensure sympathetic blockade to the arm.
A successful injection will be indicated by the rapid onset (within 5 min) of a Horner's syndrome and dilatation bf the veins in the ipsilat-eral upper limb.
Complications
1. Blockade of the phrenic nerve or recurrent laryngeal nerves. These will usually cause only minor symptoms such as hoarseness and dys-phagia, and are more common when larger volumes (20 ml) are used.
2. Intra-arterial injection into the vertebral artery can cause a major toxic reaction even with small quantities of local anaesthetic as all the injected drug goes immediately to the brain. Penetration of the arterial wall is, however, usually obvious by refluxed blood.
3. Intraspinal injection, either epidural or sub-arachnoid, can occur if the needle has entered an intervertebral foramen or the dural cuff of a cervical spinal nerve.
4. Haematoma in the neck.
Fig. 209:1.
1. Cricoid cartilage
2. Stellate ganglion
3. Middle cervical ganglion
4. Transverse process of C6
Fig. 209:3. Courtesy of Astra.
1. Transverse process of C6
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.