Fig. 49:3.
Fig. 49:4

Fig. 51:4.
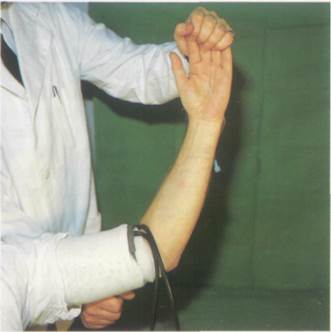
Fig. 51:5.
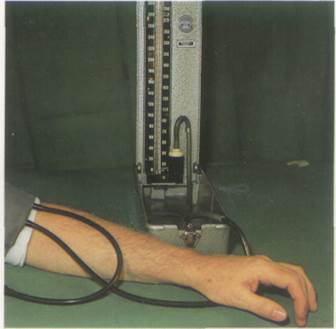
Fig. 51:2
Fig. 51:3
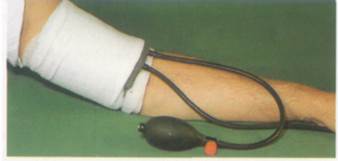

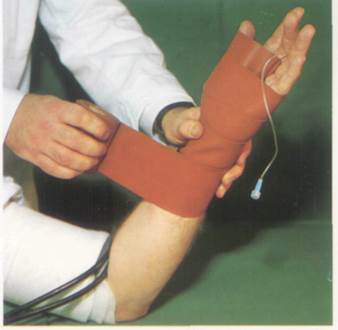
Fig. 51:6.
Fig. 51:7

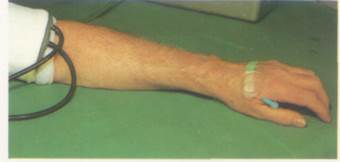
Fig. 51:8.
Lower limb
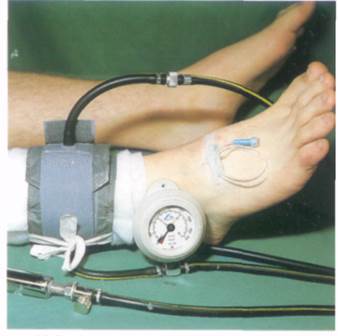
For lower limb surgery the tourniquet cuff may be placed on the thigh, the calf or the ankle (Fig. 53:1, 2 and 3) depending upon the site of the operation. An intravenous needle or can-, nula is placed in a vein on the dorsum of the foot. After exsanguinating the limb, the cuff should be inflated to a pressure of 300 mmHg or at least 150 mmHg above the systolic pressure (Fig. 53:1). The procedure is thereafter the same as for the upper limb.
Drugs and dose
With a thigh cuff the dose is 40-60 ml of dilute local anaesthetic 0.5% prilocaine, lidocaine or mepivacaine. With a calf (Fig. 51:2) or ankle (Fig. 51:3) tourniquet the dose is 30 or 20 ml respectively.
Complications
Toxicity
This may be due to accidental deflation of the cuff during or soon after injection of the local anaesthetic. Drug may also pass beneath the inflated tourniquet and reach the systemic circulation during the injection if the limb is not properly exsanguinated before inflating the cuff, and/or the injection is made too rapidly. Both can raise the pressure in the veins to levels above the pressure in the cuff. The signs, symptoms and treatment of toxicity are given on p. 22.
Tourniquet pain
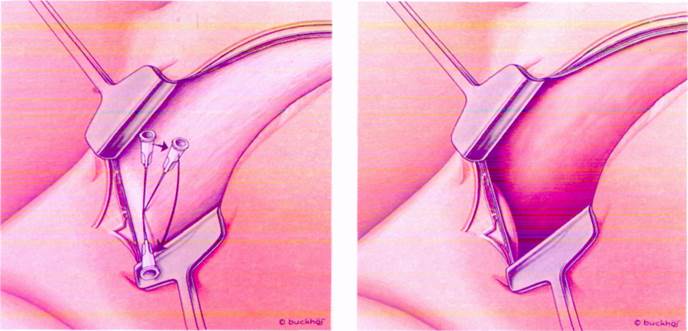
After 20 min or so the inflated tourniquet cuff may become very painful. If a second cuff is placed distal to the original one the tissues beneath it will be anaesthetised. The second cuff may then be inflated painlessly. Once the second cuff has been secured and inflated, the first one may be deflated. Specially designed double cuffs are available.
Suggested further reading:
Duggan J, McKeown DW & Scott DB (1984). Venous pressures in intravanous regional anesthesia. Regional Anesthesia 9. 70.
Holmes C.M. (1988) Intravenous regional neural blockade. In Neural Blockade, 2nd edition Cousins, M. J. & Bridenbaugh, P.O. Lippincott, Philadelphia, p. 443.
Lee A, McKeown DW, Wildsmith JAW (1986). Clinical comparison of equipotent doses of bupivacaine and prilocaine in intravenous regional anesthesia. Regional Anesthesia 11. 102.

•g 53:3

Peripheral nerve block
Regional anaesthesia of the head and neck
Most operations of the head and neck can be done under regional anaesthesia though in many cases it would not be appropriate, e.g. tonsillectomy in children. However, in the fields of dental, ophthalmological and plastic surgery, there is wide scope for the use of regional techniques, either alone or in combination with sedation or light general anaesthesia. Painful conditions, particularly trigeminal neuralgia and post-herpetic pain, can also be treated by appropriate nerve blocks.
The sensory supply to the face and the anterior two-third of the scalp is provided by the trigeminal nerve. The posterior scalp is supplied by the greater and lesser cervical nerves from the cervical plexus. The anterior neck receives the transverse cutaneous nerve of the neck~ which derives from the anterior primary rami of C2 and 3, as does the greater auricular nerve supplying the skin of the external ear and the skin below it. The posterior rami of C3, 4 and 5 supply the skin of the back of the neck.
The motor supply is from the facial nerve, which supplies the muscles of the face, and the trigeminal nerve which supplies the muscles of the mastication.
Trigeminal nerve block
Anatomy
The trigeminal nerve is the largest cranial nerve (Fig. 57:1). It is formed by the union of a sensory and a motor root. At the point of this union is the trigeminal (Gasserian) ganglion, which lies within the cranium in a depression close to the apex of the petrous part of the temporal bone. Through its three main branches it supplies the skin of the face and scalp, and the muscles of mastication (Fig. 57:2).
The three branches are:
1. The ophthalmic nerve, which leaves the cranium through the superior orbital fissure
2. The maxillary nerve, which leaves through the foramen rotundum
3. The mandibular nerve, which leaves through the foramen ovale
Уважаемый посетитель!
Чтобы распечатать файл, скачайте его (в формате Word).
Ссылка на скачивание - внизу страницы.